
Surviving a Difficult Rotation in Anatomical Pathology Residency
Everyone knows that medical residency is not for the faint of heart. It is not a 40-hour workweek, with scheduled lunch and coffee breaks, and it does not have the comfort of regular hours. Nor does the work stop when you get home—in fact, you are likely to be catching up on patient notes or on reading and studying for your rounds and exams.
When it comes to difficulty, a residency in anatomic pathology is considered to be on the easier end of the spectrum. The hours are better, or so it is said. Compared to our friends in clinical specialties, it’s true that you don’t have to be in clinic to see patients at a specific time. Also, at least at McGill, there are few very strict demands on when a resident needs to be in (e.g. covering intraoperative consults). The fact that is very rarely discussed is the amount of studying involved, and that level of studying really takes time, so my personal experience thus far is that just studying accounts for a lot of hours in addition to service work. Then there’s also the fact that studying for the Royal College exams (corresponding to medical licensure exams in Canada) is a whole lot different from studying for cases routinely seen in service on subspecialty rotations.
But I digress. The point that I am trying to make is that anatomic pathology residency, however enjoyable, is certainly not a walk in the park.
In fact, there are a few rotations in anatomic pathology residency at McGill that have been recognized across several residency batches as difficult. Residents have given various reasons for a rotation being difficult, but the most common reasons are the following:
- The staff are horrible and can wreak emotional havoc if you don’t steel yourself and take care of your mental health;
- The workload is more than usual, with lots of cases or full service assigned to residents, and with grossing and/or administrative work (EPAs, I’m looking at you) and other duties involved.
- The specific subspecialty rotation is simply boring and uninteresting (for them), and it’s difficult to make an effort.
So how can one survive, and ideally thrive, in a difficult rotation in anatomical pathology residency?
Workload Management
- Stay (very) organized. Keep a detailed logbook of cases grossed, seen, your preliminary diagnosis, and the official signout. Take notes of your attending’s teaching points. This logbook is important especially if you’re working with different staff (I used to keep one spreadsheet per staff) and you’re asked for updates (e.g. what stains have come in). This will also be useful in tracking your progress in terms of evaluations and learning exposure.
- Ask for help! Don’t hesitate to consult with your co-residents when faced with challenging cases. As a side note, check with your attending before showing a case to another staff pathologist, in case an official intradepartmental referral is necessary. Trust me on this, you just don’t want to ruffle (delicate) feathers. Asking for help also means requesting assistance from support staff (pathology assistants, lab managers, technicians). The more of them you befriend, the easier and more enjoyable working will be.
- Figure out a schedule that works for you. By now you should have a good idea of when your most productive hours are, how long you can work, how many breaks you need. Combine this with the responsibilities that you have and see if you can figure out a schedule that maximizes your personal efficiency. For example, the pediatric pathology rotation at McGill required that we gross all big (and sometimes medium) cases, take full service responsibility of intraoperative consults, biopsies, and resections, and also be in charge of weekly rounds and tumor boards. I took these into consideration, as well as the fact that I lived far from the hospital and would rather avoid rush hour traffic, my attending’s preferences for daily signout, and my own strong ideas about not coming in during weekends to work. That said, I set up a schedule where I was in at 6 AM, previewed the most difficult cases first, looked at possible intraoperative consults at 8AM, reviewed cases with staff at around 11AM, grossed big cases in the afternoon and saw more cases or did my background reading, and did secretarial work like logbooks in the evening. Most days I was out by 6 PM. Sometimes, if there were many small cases to gross, I did this late into the night (like 10 or 11 PM), especially if I was on call anyway. I tried to do all digital presentations a week in advance, scanning slides when necessary, and finished these the weekend prior. This worked for the entire 3 months of my rotation, did not cause me any burnout, and my exit evaluation was satisfactory.
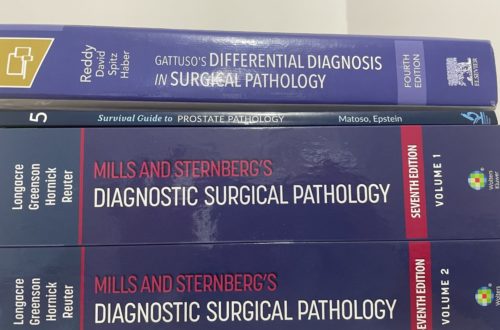
- Choose only a few major references and stick to it. There are a lot of great references available in pathology, and I know a lot of residents look up information on the fly while looking at a case. I am a big fan of Kurt’s Notes for a lot of rotations, but a deeper understanding of how concepts are interconnected or even an approach to an organ system may require an actual textbook. For hematopathology, for example, for non-neoplastic entities my go-to was that one chapter in Jaffe. For neoplastic hematopathology, I found Survival Guides extremely helpful, and for details I just used the WHO bluebook. For this two-month rotation, I was not really tempted to seek out other references, such as Ace the Boards or the rest of Jaffe, as I needed something digestible but with some depth. If I had wasted time flip-flopping from one resource to another, I feel like the information would not have been as organized in my brain as it is right now.
Mental Health and Well-Being
All of the aforementioned tips seem to be all about work, but we know that is usually a recipe for burnout. So how do we care for ourselves even during the most difficult rotations?
- Take breaks at work. Make sure you eat, look away from the scope to rest your tired eyes (no matter how ergonomic your setup is), and even chat for a bit with friends.
- Maintain work-life balance (as much as you can). Set boundaries and make time for activities outside of work. For busy rotations, I consider my weekends and evenings sacred and just for family and personal hobbies. When I am not on call, I do not even answer text messages or (ugh) phone calls from staff outside of reasonable working hours, unless a previous appointment has been arranged.
- Practice self-care, even though it sometimes feels like a burden and it does not contribute to productivity. This means prioritizing sleep, exercise, and healthy eating habits. I was guilty of snacking so much during difficult rotations just to stay awake, so don’t be like me! Or at least have healthy snacks on hand. Ask a co-resident (or two) to take a walk with you inside or outside (around) the hospital. When there is an opportunity for sleep, take it instead of doomscrolling. Although, to be honest, if it’s a really exhausting rotation, I just zonk out when I reach home.
- Take days off if possible. During busy rotations, sometimes it just so happened that I have had to take my daughter or myself to health appointments, which necessitated taking days off. I used those days to spend more time with family and recuperate or to catch up on some work and studying if I really need to. In retrospect, those catch-all days were not “off” in the strictest sense of the word, but they also helped me keep my mental health in great shape.
- Strengthen your emotional support network. To me, this meant spending as much time as possible with family, chatting once in a while with friends outside work, and even having armchair conversations with co-residents.
- Outsource as much as you can. This is probably the most underrated tip ever. I know not everyone has the capacity to do this, but whatever you can delegate, just delegate. During rotations that required more of my time, my husband took a few hours from work to make sure he could spend time with our daughter and tend to our home. We hired cleaners, we purchased food from caterers. I also asked for a lot of help from family and in-laws.
Maximizing Learning
Some people say that the harder a rotation is, the more you learn. This may be true, may be an excuse given by harsher physician staff, or may just be a consolation resident tell themselves to get through the long days (and nights). What is definitely true, however, is that any rotation is an opportunity for educational advancement in the specialty you have chosen.
With these tips for surviving a difficult rotation in pathology, it is my hope that I have helped you brace your shoulders, adjust your mindset, dismiss errant traits in attendings and the humdrum of scutwork as mere distractions, so that you can keep your eye on the prize: learning as much as you can and becoming the best pathologist you can be.




2 Comments
PathologyResident
I am wondering if you could comment on how you use handwritten notes? This is something I’ve always preferred but people have always said it’s too time consuming or not practical to handwrite notes from textbooks, i.e. Robbins. I am a PGY1 and just trying to figure out how to go about writing notes on textbooks, or whether I should type them!
Dr. Jade Marie Tomaszewski
Hi! I admit I have never really taken notes by hand when reading our large textbooks (e.g. Sternberg, Robbins), as to do it would indeed be time consuming. I do take handwritten notes during signouts (using pen and paper or my iPad) and transfer them to Notion (so I can review them more easily). For heavier books, I used to do a highlight, and then copy-paste important tables and/or rewrite concepts in Notion. Nowadays what I do for digital books is that I use Zotero, which allows me to annotate (even with handwriting!) and access the file on Windows and Apple. Oh, and I write handwritten flashcards on Feyn because it fits and looks nice on my phone too. So basically I handwrite across a lot of programs on my iPad and also with pen and paper, digitize as a form of review, and centralize as much as possible on Notion and Zotero. Hope this is helpful!